Menopause brings widespread physiological change as the body adjusts to new hormonal rhythms. One of the most recognizable and disruptive effects of this transition is hot flashes, which are sudden waves of heat that spread through the chest, neck, and face, often followed by sweating, chills, and a pounding heartbeat.
Hot flashes affect roughly 80% of women during and after the menopausal transition.1 For many, they continue for years, interrupting sleep, daily activities, and quality of life. Hormone replacement therapy (HRT) has long been the conventional approach, yet not everyone can or chooses to use it, leading researchers to explore other ways to ease these symptoms.
A recent clinical trial published in JAMA Network Open tested a simple, self-directed method rooted in hypnosis — a mind-body practice that uses guided relaxation and imagery to influence physical responses. The study opens new ground in understanding how focused mental states may help stabilize the body’s shifting internal balance during menopause.2
What Are Hot Flashes and Why Do They Occur?
In menopause, the hypothalamus, which acts as the body’s thermostat, becomes unusually sensitive to even minor fluctuations in core temperature, treating small rises in body heat as signals of overheating. The result is a cascade of physiological reactions aimed at cooling the body. These temperature-related reactions are classified as vasomotor symptoms, referring to the changes in blood vessel tone and circulation that drive both hot flashes and night sweats.3,4
• Vasodilation produces a sudden wave of heat — When a hot flash begins, blood vessels near the skin’s surface dilate rapidly, a process called vasodilation. This rushing of blood to the skin’s surface creates the characteristic sensation of heat and causes visible flushing. Heart rate may also increase by 7 to 15 beats per minute.
• Sweating follows as the body’s primary cooling mechanism — Sweat glands respond aggressively, sometimes producing enough perspiration to soak clothing or bedding. As the sweat evaporates, it lowers body temperature — sometimes too abruptly — leading to chills or shivering once the episode subsides.
• Duration and frequency vary widely — Hot flashes typically last between 1 and 5 minutes. Some women experience only a few per week, while others may endure 20 or more daily. The intensity also differs, ranging from mild warmth to intense heat that interrupts normal activity.
• Environmental and lifestyle triggers amplify symptoms — Warm rooms, spicy foods, caffeine, alcohol, stress, and tight clothing can all provoke hot flashes in susceptible individuals. Identifying and avoiding personal triggers often helps reduce frequency and intensity.5
• Night sweats disrupt sleep and recovery — When hot flashes occur during sleep, they are called night sweats. These can cause sleep disturbances and lead to fatigue, mood changes, and poor concentration over time.6
• New research challenges the estrogen-deficiency model — Hot flashes have long been attributed to a decline in estrogen, a view that has shaped decades of conventional menopause treatment. However, emerging evidence suggests this interpretation oversimplifies a far more complex hormonal landscape.7
A 2024 study published in The Journal of Clinical Endocrinology and Metabolism found that many menopausal women do not have low estrogen throughout the body. Estrogen often remains elevated in tissues such as fat, even when blood tests suggest a decline. What declines more substantially is progesterone, the hormone that counterbalances estrogen’s effects.8
This shift creates a state of relative estrogen dominance rather than deficiency. Related findings also showed that key protective hormones like progesterone, thyroid hormone (T3), pregnenolone, and DHEA steadily declined with age.9 You can learn more about this in “Menopause and the Influence of Estrogen Dominance.”
This understanding challenges the routine use of HRT as a corrective measure. If estrogen activity is already high in tissues, adding more may deepen the imbalance rather than restore equilibrium. Against this backdrop, the study on self-hypnosis as a nonhormonal method for easing hot flashes gains even greater relevance, offering a way to address these symptoms without further disrupting hormonal stability.
Study Shows Self-Hypnosis Significantly Reduces Menopausal Hot Flashes
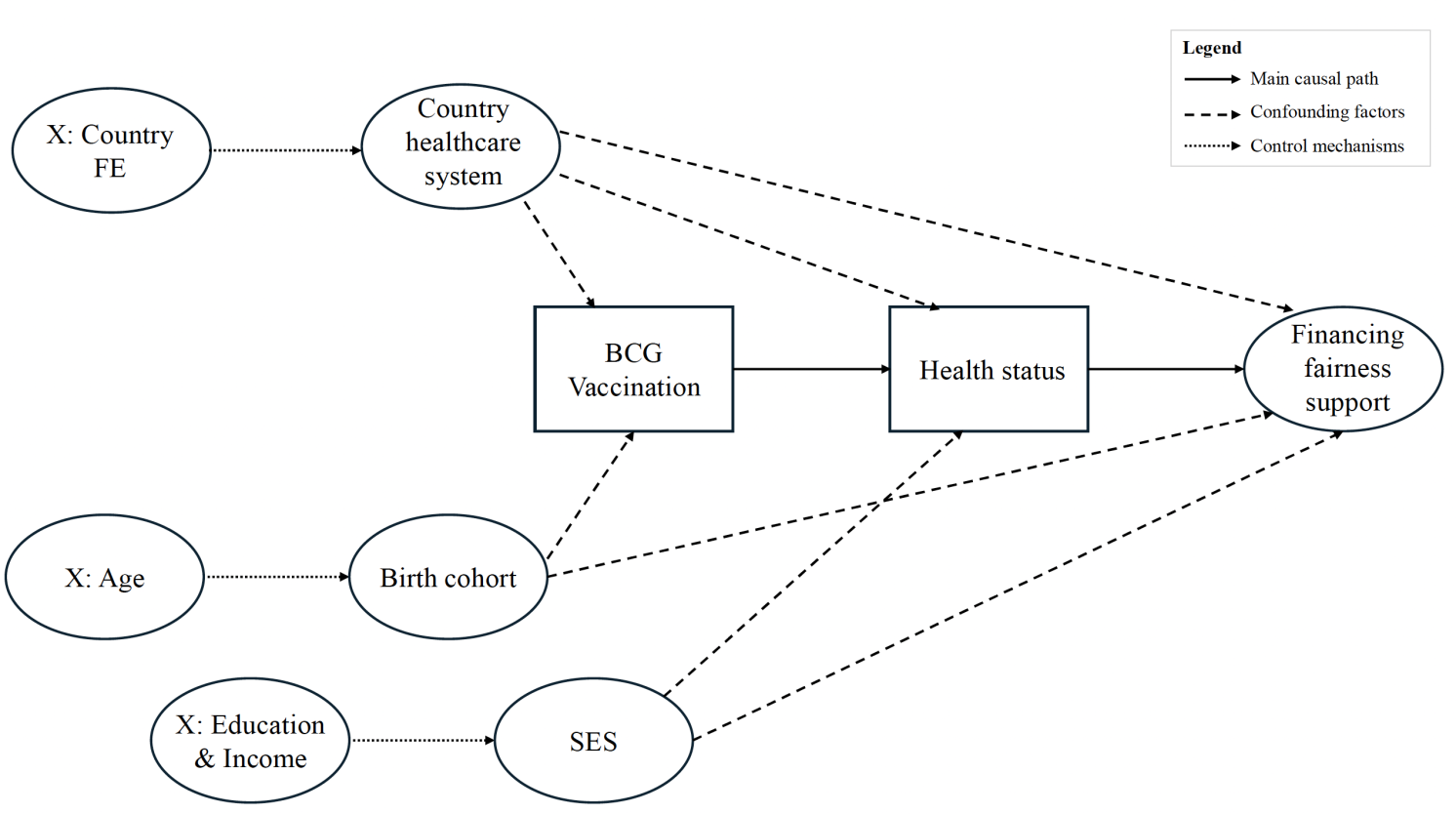
The featured study, led by researchers from Baylor University and the University of Michigan, was structured to distinguish the true physiological effects of hypnosis from placebo responses. The study enrolled 250 women experiencing at least four hot flashes daily or 28 weekly, including 62 women who were breast cancer survivors, a group that often experiences more severe vasomotor symptoms and cannot safely use hormone-based treatments.10
• Participants were randomly assigned to one of two groups for six weeks — The intervention group received daily audio recordings guiding them through a 20-minute self-hypnosis session combining relaxation, focused attention, and mental imagery of coolness. These techniques are aimed at influencing the body’s thermoregulatory system through mental focus.
Meanwhile, the control group received “sham hypnosis,” consisting of white noise recordings labeled as hypnosis, accompanied by the same educational materials. Both groups were asked to practice daily and log their sessions in a diary. This design matched for time, expectation, and engagement, isolating the effects of hypnosis content itself.
• Symptom tracking and outcome measures — Hot flashes were recorded using validated daily diaries that captured both frequency and severity, yielding a composite hot flash score. Participants also completed the Hot Flash Related Daily Interference Scale (HFRDIS) to measure how much symptoms affected sleep, mood, concentration, work, and social life, as well as a global improvement scale rating perceived benefit.
• Reduction in hot flashes and symptom severity — Women practicing self-hypnosis achieved a 53.4% reduction in hot flash scores at six weeks, compared with 40.9% in the control group. By week 12, reductions reached 60.9% versus 44.2%. Among women who completed the study, 60.4% of those practicing hypnosis achieved at least a 50% reduction in hot flash scores compared with 42% in controls.
The intervention proved most effective for moderate hot flashes, decreasing from 21.6 per week at baseline to 8.0 at week six and 7.8 at week 12, while the control group improved from 20.9 to 12.5 and plateaued. Severe episodes also declined sharply from 6.1 to 1.3 per week in the hypnosis group, compared with 6.8 to 3.8 in controls.
• Marked improvement in daily functioning — Hot flashes interfere with many aspects of daily life, and the hypnosis intervention substantially reduced this burden. HFRDIS scores fell 49.3% in the hypnosis group versus 37.4% in controls. The largest improvements occurred in leisure and enjoyment of life, which decreased by 62.6% in the hypnosis group compared with 51.3% in controls.
• High satisfaction and strong adherence effects — When asked to rate overall benefit, 90.3% of women using self-hypnosis rated themselves as “a little better,” “moderately better,” or “very much better,” compared with 64% in the sham group. One-third described their symptoms as “very much better,” nearly twice the proportion seen in controls. Women who practiced daily achieved the greatest symptom reductions.
• Notable benefits for breast cancer survivors — The 62 breast cancer survivors in the trial began with higher baseline symptom severity but showed the largest treatment gains. Their average composite hot flash scores dropped from 98.2 at baseline to 35.4 after six weeks (a 64% reduction), while scores in the control group declined from 84.7 to 54.6.
By the trial’s conclusion, self-guided hypnosis produced clinically meaningful and sustained reductions in both the frequency and severity of menopausal hot flashes. The parallel improvements in quality of life, combined with the absence of risk, identify this low-cost, nonhormonal strategy as a viable option for managing vasomotor symptoms, particularly for women who cannot or prefer not to use HRT.
Additional Strategies to Manage Menopausal Symptoms
While hypnosis has demonstrated clinically significant effects on hot flashes, other approaches offer varying degrees of relief for menopausal symptoms. Roughly half of menopausal women use at least one nonhormonal approach, and most report some degree of benefit. The following mind-body practices, natural products, and whole-system approaches have been studied for relief of menopausal symptoms:
• Cognitive behavioral therapy (CBT) — CBT focuses on identifying and changing unhelpful thought patterns and behaviors that amplify symptom distress. Trials among menopausal and breast cancer survivor populations show CBT can meaningfully reduce how disruptive hot flashes feel, even if it doesn’t lower their actual frequency.
Women who participated in structured four- to six-week CBT programs reported reductions of 48% to 52% in perceived interference from vasomotor symptoms. CBT also improves mood and coping, helping women feel less overwhelmed by sleep problems and emotional fluctuations.11
• Relaxation and biofeedback training — Progressive muscle relaxation, guided imagery, and paced breathing teach better control of the body’s stress and temperature responses. In several clinical trials, women practicing applied relaxation reported up to a 55% drop in hot flash frequency after 12 weeks.
Biofeedback uses sensors to track skin temperature or heart rate to help reinforce awareness of early heat signals, allowing users to calm these reactions before they intensify. Although findings are not uniform across studies, relaxation-based methods are low-risk and may ease both vasomotor and psychological symptoms.12
• Mindfulness-based stress reduction (MBSR) — This approach typically involves an eight-week structured program that combines mindfulness meditation, gentle yoga, and breathing awareness. Research shows that while MBSR does not significantly reduce the number or intensity of hot flashes, it improves sleep quality, lowers anxiety, and enhances overall quality of life by promoting present-moment awareness and reducing stress sensitivity.13
• Yoga — Evidence suggests modest benefits for psychological well-being, fatigue, and sleep during menopause. In one 12-week trial, yoga improved scores on the Menopause Rating Scale and quality-of-life measures. Differences in yoga style and intensity likely influence outcomes, but overall, yoga appears safe and supportive for mental and emotional balance.14
• Aromatherapy and massage — Inhalation of lavender aromatherapy for 12 weeks improved sleep quality and reduced anxiety in menopausal women. Another study found that lavender essential oil cut hot flash frequency by 50% compared with less than 1% in placebo. When paired with massage, aromatherapy further improved mood and physical comfort, offering a calming sensory intervention for stress-related symptoms.15
• Herbal and nutritional approaches — Several plant-based and nutritional therapies have been explored for their ability to ease menopausal discomfort and support general well-being, though further studies are needed to confirm consistent benefits. These include:16
◦ Black cohosh — An herb native to North America, traditionally used for women’s health, black cohosh has been shown in some studies to reduce hot flash severity by up to 50%.
◦ Maca — A root vegetable from the Andes, maca is valued for its adaptogenic properties and has been linked to improvements in mood, energy, and sexual function.
◦ Dong quai and evening primrose oil — Dong quai, often called “female ginseng,” has long been used in Chinese medicine to balance hormones and circulation. Meanwhile, evening primrose oil, derived from the seeds of the evening primrose plant, supports skin and nerve health and may offer mild relief from vasomotor symptoms.
◦ Vitamin E — A fat-soluble antioxidant that supports cellular and cardiovascular health, vitamin E supplementation has been associated with modest decreases in hot flash frequency in some studies.
• Acupuncture and reflexology — Acupuncture has been widely studied, with some trials showing improvements in vasomotor and sleep symptoms. Foot reflexology, a type of massage targeting specific pressure points in the foot, has reduced hot flashes by over 50% in some studies and improved sexual function and mood.17
• Sauna therapy — Regular sauna use supports metabolic health during menopause by enhancing insulin sensitivity, improving circulation, and promoting efficient fat metabolism. These effects may help counter the gradual weight gain and metabolic slowdown that often accompany hormonal shifts.18 Read more about this approach in “Daily Sauna Use May Help Menopausal Women Avoid Weight Gain.”
• Progesterone support — Three hormones that most adults can benefit from are progesterone, DHEA, and pregnenolone. For perimenopausal and menopausal women, progesterone is especially useful.
In one study, progesterone supplementation significantly improved night sweats and sleep quality among perimenopausal women.19 If you’re considering this option, I explain how to use progesterone safely and effectively in the section below.
Frequently Asked Questions (FAQs) About Menopausal Hot Flashes
Q: What exactly happens in my body during a hot flash?
A: During menopause, your hypothalamus, which acts as the brain’s internal thermostat, becomes oversensitive to small changes in core temperature. When it mistakenly detects overheating, it triggers vasodilation, which sends warm blood toward the skin’s surface, followed by sweating to cool the body down.
If the body cools too quickly, you may feel chills. These rapid shifts in circulation and temperature are what define vasomotor symptoms such as hot flashes and night sweats.
Q: How does self-hypnosis reduce hot flashes?
A: Self-hypnosis works by calming the nervous system and influencing the body’s thermoregulatory center. In the JAMA Network Open clinical trial, participants listened to daily audio recordings that used guided relaxation and imagery of coolness. This process helped stabilize temperature perception, reducing both the frequency and intensity of hot flashes.
Q: Is self-hypnosis safe to try on my own?
A: Yes. In the study, women practiced safely at home using audio guidance without therapist supervision. Start by setting aside 20 minutes each day in a quiet space. Choose recordings specifically designed for menopausal symptoms. If you prefer professional guidance, a certified hypnotherapist can help you learn the technique before continuing independently.
Q: How long does it take for self-hypnosis to work?
A: Most women began noticing improvement within a few weeks of consistent use. The greatest benefits appeared around six to twelve weeks. The more regularly you practice, the stronger the effect. Daily sessions create the most lasting results.
Q: What other nonhormonal options might help me manage menopause symptoms?
A: Evidence supports several complementary approaches. Cognitive behavioral therapy (CBT) can reduce how disruptive symptoms feel and improve coping. Relaxation techniques and biofeedback help regulate stress and temperature responses. Yoga and mindfulness improve mood and sleep, while aromatherapy, acupuncture, and reflexology provide additional comfort and stress relief.



Leave a Reply